Digital health is poised to bring its disruptive force across the healthcare landscape, and the pharmaceutical industry isn’t immune to the upcoming changes. Turning the point of care towards patients and empowering them with their health data, this cultural transformation brings about a radical shift in the traditional functioning of the drug industry.
In our latest e-book, the Medical Futurist team analysed 11 of the major digital health technologies and practices with the greatest impact in this sector. From including patients in decision-making through personalised care to automating pharmaceutical processes, we compiled our findings in this new e-book.
Those who embrace the paradigm shift that digital health brings about will be better prepared for the upcoming changes in pharma. Moreover, those companies will get a head start as compared to competitors. To learn more, you can get your own copy of “Technologies Shaping The Future Of Pharma” on LeanPub below:
In this article, we share 5 take-home messages from the e-book that the new wave of digital health is bringing into pharma. If these pique your interest, we encourage you to dive deeper into these topics and more in the full e-book!
1. Patient inclusion in key decision-making processes improves deliverables in pharma
For as long as the drug industry has existed, patients’ roles have revolved solely as the end-user; destined to use products which were years in the making. However, all steps that had occurred prior to obtaining the finalised product happened within the heavily-guarded doors of pharma’s ivory tower. With 21st-century technologies, these doors burst open and patients made their way into the proverbial tower.
A prime example is that of the “#wearenotwaiting” movement created by diabetics. The latter, fed up with lagging regulations that kept MedTech companies from introducing an artificial pancreas into the market, took matters into their own hands. Through online communities, they created such an open-sourced DIY pancreas. They further built discussion platforms like DiabetesMine and cloud-based solutions like Tidepool for more accessible and actionable diabetes data. Their initiative even forced the FDA’s hand to later approve the first commercial artificial pancreas.
This exemplifies the need for pharma authorities to include patients in their decision-making processes. Through their input, their exact needs will be known and better products will be delivered to attend to these needs.
It’s not enough to have patients fill out surveys as part of “patient centricity”. What pharma companies need to adopt is patient design. It goes beyond the passive act of asking about their opinion and actively involving them in crucial steps that will impact their health.
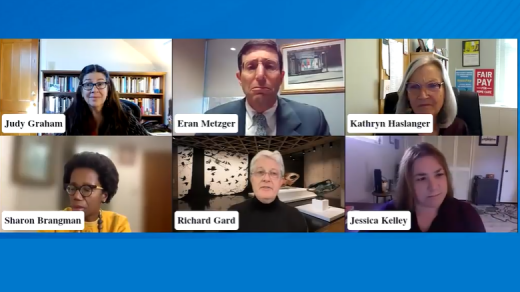
In 2017, the FDA held its first Patient Engagement Advisory Committee meeting. It set the pace to involve patients in their regulatory activities. The European Federation of Pharmaceutical Industries and Associations (EFPIA) also took steps in this direction. It developed a framework to integrate patient organisations in their decision-making. Other members of the pharmaceutical industry could adopt similar strategies in order to better attend to their patients’ needs. In addition, such approaches will help deliver appropriate solutions in a timely manner.
2. Integrating AI in drug development slashes time and cost
From finding suitable candidates for animal trials, from unexpected side effects in clinical trials to multiple trial-and-error sequences, drug development is understandably a lengthy and costly process. In fact, estimates put the numbers at about 12 years and an investment of between $1 billion and $2.8 billion for an experimental drug to advance from a lab to the market.
However, developments in the field of artificial intelligence can now help diminish the cost and time traditionally associated with drug development. To exemplify this possibility, Insilico Medicine, an AI pharma startup, identified a potential new drug in only 46 days. Its algorithm achieved this by analysing vast amounts of data which would otherwise take humans years to go through. The drug didn’t result in a commercial one as this achievement was to prove the potential of AI in drug development. However, practical examples do exist within the industry.

Partnering with IBM and the University of Toronto in 2015, AI startup Atomwise used its algorithm to identify two drugs with significant potential to reduce Ebola infectivity. It accomplished this effort in less than a day. In 2020, the company teamed with researchers to find broad-spectrum treatments for COVID-19 and future coronavirus strains.
Also concerning the COVID-19 pandemic, the BarabasiLab paired its network medicine toolset with AI to find potential treatments. The team managed to obtain a list of such drug candidates in less than 10 days. The latter is undergoing tests on human cell lines in experimental labs. These are only a few examples of drug companies employing AI’s benefits in drug development. In fact, there are hundreds of startups and this number will only keep climbing.
To illustrate the speed of development, we only have to look around for some recent examples. Scientists used a new type of computational method that allows them to computationally test billions of compounds against a therapeutic target. As described in their Nature paper, they tested 11 billion theoretical compounds against a cannabinoid receptor (CB2) that marijuana’s active ingredient THC targets.
And this is just the beginning! As I always say, one of the most progressing areas of AI’s potential in healthcare lies in drug design. Maybe this is the field that we could call the low-hanging fruit of the AI revolution.
Look at this announcement: “In a paper that will be presented at the International Conference on Machine Learning (ICML), MIT researchers developed a geometric deep-learning model called EquiBind that is 1,200 times faster than one of the fastest existing computational molecular docking models, QuickVina2-W, in successfully binding drug-like molecules to proteins.”
No genius drug researcher can compete with something being 1,200 times (!) faster than not him/her, but the previous supercomputer model.
3. With 3D printing, pharma companies can make personalised medicine a reality
Despite being a relatively new technology adopted in healthcare, 3D-printed drugs show great promise. The first FDA approval of a 3D-printed pill was issued only in 2015, but the technology already paves the way for personalised medicine. This was, in fact, the conclusion of a 2019 research. The researchers involved successfully 3D-printed 6 different drugs into a single, multilayered polypill. With this technique, pills of specific doses tailored to individual patients are made possible.
Medical 3D-printing company FabRx is aggressively working towards this goal. In April 2020, they released M3DIMAKER – the first pharmaceutical 3D printer to manufacture personalised medicines. It allows for the printing of medicines according to the user’s manufacturing needs, which in some cases means one month’s medication (28 pills) in around 8 minutes!
Traditionally, pills were manufactured in standard doses and had to be manually adjusted, for example, by crushing or splitting them in order to fit the dose for children. This method potentially leads to dosage errors or even improper drug use. With M3DIMAKER, this issue is a thing of the past. The printer allows pharmacists to make pills with precise doses for individual patients. “I truly believe that we are one step closer to personalised medicine thanks to the M3DIMAKER,” said Dr. Alvaro Goyanes, Director of Development at FabRx.
4. Boosting adherence of chronic care patients with digital pills
Yearly, lack of adherence to one’s medication amounts to 125,000 deaths and around $300 billion in healthcare costs; all of these are in fact preventable. Other reports paint an ever grimmer picture, estimating a $500 billion impact, with non-adherence showing a significant correlation with the cost of the treatment.
However, adhering to treatment plans with multiple medications is especially challenging for patients suffering from chronic conditions such as schizophrenia or cardiovascular diseases. To remedy this pressing issue, digital pills can boost adherence while preventing deaths.

The FDA first approved such a digital pill in 2017 produced by Otsuka Pharmaceutical and Proteus for chronic mental disorders. This pill contains an ingestible sensor which is a wearable patch sensor and an app track. This allows physicians to monitor a patient’s compliance with the treatment.
Although Proteus filed for bankruptcy in June 2020, the technology it employed isn’t at fault. The digital pill field was born, and there are a number of interesting players.
Digital health company etectRx aims to advance patient medication adherence and improve ingestion tracking technology. The company’s flagship product, the ID-Cap System is an ingestible event marker: a gelatin capsule with an ingestible sensor that transmits signals to a wearable reader, which sends the data to a smartphone-based app and secure cloud-based server to enable reliable tracking of ingestion events.
Harry Travis, CEO and President of the company told The Medical Futurist in an interview that they had three NIH-funded research studies underway (at the time of the interview), and had completed an HIV-prevention study with Brigham and Women’s Hospital in partnership with The Fenway Institute at Fenway Health in Boston, in which their technology recorded medication ingestions with 98 percent accuracy.
The pandemic also highlighted the importance of remote control over medication adherence, and many trials moved towards monitoring patients remotely instead of requiring in-person visits to a clinic.
5. Automation supplements the supply chain with more effective solutions
With automation, repetitive manual tasks are a thing of the past. By including robots in drug-manufacturing factories, the supply chain gets a boost in effectiveness. These automated machines are rapid and consistent with the task programmed while being cost-effective.
Such solutions already are in practice in the industry. Denso Robotics supplies pharmaceutical robots for manufacturing processes, while Innovation Associates offers PharmASSIST ROBOTx, an automated dispenser. The latter’s dispensing capacity range is scalable and its data mining ability allows pharmacists to optimise its use based on these insights. Already in Denmark, 70% of community pharmacies already use such automated dispensing robots. In mainland Europe, 30-40% of pharmacies use these solutions.
A growing concern with automation is that of not requiring human assistants, leading to rising unemployment. However, the opposite might be true. A pharmacist in Scotland employed more people after including automated technologies in the pharmacy; the reason being the need for more people to manage the resulting increased turnover with automation.
Moreover, with mundane, repetitive tasks delegated to robots, human input will be important in responsibilities requiring creativity and problem-solving skills. Technology also lends a hand in these situations. Training of workers can be enhanced with augmented reality by overlaying useful instructions in the real world. For manual workers dealing with heavy weights or standing for long hours, exoskeletons provide additional support.
As such, drug companies stand more to gain by integrating automation into their supply chain than by shying away from it.

As we come to the end of this article, we hope that the topics discussed here have got you interested in learning more about how digital health technologies shape the future of pharma. We again invite you to read our analysis in our latest e-book on LeanPub. We look forward to your feedback!
The post Technologies Shaping The Future Of Pharma e-Book appeared first on The Medical Futurist.