by Joe Maher, CPA, MBA
Editor’s note: Matt Ritzert, Senior Consulting Director, Sg2, contributed to this post.
Clinically integrated networks (CINs) gained a foothold more than a decade ago amid the backdrop of an unsustainable trajectory for fee-for-service (FFS) health care delivery. CINs could function as a vehicle for value-based care (VBC) models in providing an alternative for clinical and payment model advancement. Since then, CINs have become a cornerstone of care delivery, enabling clinical value creation and economic value capture. Looking back on the evolution of CINs provides both key learnings and insights on how CINs are likely to deliver even greater value.
In 2023, Vizient is releasing a publication offering an in-depth review of lessons learned through the early iterations of CINs. The journey has been marked by encouraging progress and growth as well as by ongoing challenges that will need to be navigated. This publication will provide a point of view on where the next iteration of CINs (CIN 3.0) are likely to develop and evolve. Meanwhile, this post highlights a few concepts that the piece will explore in more depth.
CIN 1.0—learnings from the first iteration
In an era defined in part by the Affordable Care Act, CINs gained momentum as a vehicle for provider organizations to work together in advancing clinical care, quality and outcomes. These entities could jointly contract with payers to align financial incentives based on value. CINs have proven durable in engaging providers and systems in value-based care. Beyond the core VBC focus, CINs have provided organizations a provider and delivery alignment mechanism that allows entities to legally work together while maintaining independence.
Early in the journey, it became apparent that CINs would face wide variation in physician alignment, which persists today. CINs were able to engage primary care providers (PCPs) in both creating clinical value and incentivizing value capture. Despite elevating PCPs in the journey, nearly all CINs continue to struggle to engage specialists.
There was early optimism that CINs would help spark a more rapid transition, but it became apparent that transition to VBC would take time. Fortunately, CINs built momentum by renewing focus on delivering clinical value.
CIN 2.0—where the journey has brought us
Many CINs with sufficient tenure have made significant progress in the value-based care journey. This success is underscored by the increased number of lives in VBC contracts, often spanning all payer classes. The evolution from CIN 1.0 to CIN 2.0 is best marked by the shift to the cost side of the value equation. The financial upside of shared savings and other total-cost-of-care arrangements further elevated engagement when CINs were able to share more materially in the financial upside of VBC.
With additional apparent financial upside, CINs have become more willing to invest in VBC opportunities. A corresponding challenge has been evaluating ROI, which is considerably more complicated in VBC than in FFS. Value-based care horizons are longer (often greater than one year) and more difficult to measure. Two areas CINs must continue to advance to promote VBC ROIs are (1) effectively integrating data and (2) increasing stakeholder understanding.
Many CINs have robust data from multiple sources, and like most in the industry, CINs struggle to effectively integrate the data to drive accountability and change. At the same time, CIN leaders are working across constituent stakeholders to educate on how VBC investments and returns should be understood. With a number of success stories to lean on, CIN leadership and governance is equipped to reach more broadly within and across organizations. Better data and credible ROIs will continue to help bolster this engagement.
CIN 3.0—key traits among CINs taking the next big step in value-based care
With value-based care gaining broader adoption, CINs have another opportunity to serve as clinical and economic engines for VBC. In most cases, this evolution will require advances in the care delivery model, the financial model and the operating model.
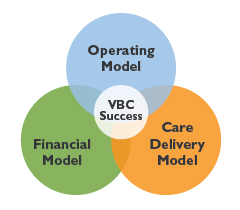
Value creation in the care delivery model will blend larger-scale adoption of best practices and integration of more modern technology-enabled care delivery solutions.
High-value pathways pioneered by multiple providers and delivery systems will become commonplace. Clinical pathways will help reduce variation in the practice of medicine, which in turn will contribute to reduced cost variation. CINs will bring a focused approach to reducing and removing non-value-added care.
Because the care received by a small proportion of patients expends an outsized proportion of health care delivery resources, CINs will focus on more effectively reaching these higher-cost populations. This approach will include deploying patient activation resources and technology tools to support the patients outside of the clinical setting, particularly for patients with chronic conditions. The impact will be especially pronounced with the emerging importance of home-based care delivery.
Value capture in the financial model will require a portfolio-level view that reflects an understanding of financial risk and even strategically leverages downside.
CINs entering this next phase of maturity will have significant financial responsibility and upside opportunity for attributed lives across payer classes. Key decision makers will continue to bring a strong understanding of total-cost-of-care management approaches, including the nuances of a multiyear horizon coupled with inherent variation.
Many CINs have been cautious in undertaking any downside financial responsibility. While caution is appropriate, downside avoidance will be limiting. As such, downside risk conversations will move from a binary “either-or” concept to a strategic lever that should amplify upside opportunity. Downside risk can enable greater value capture on the upside. It will also demonstrate CIN commitment and focus that promotes accountability related to total cost of care.
CIN infrastructure will become more intertwined and embedded in the strategic aims of health system infrastructure as value-based care opportunities become more prominent.
With FFS headwinds and fewer growth opportunities on the horizon, health systems are likely to become more interested in VBC, as it affords new margin opportunities. Given the infrastructure and expertise that reside within advanced CINs, they will become strategically essential to the success of the CIN model.
At the same time, further investments will be needed to ensure continued growth. Technology tools and capabilities to run the networks will be critical. Similarly, investments in people will be essential, including recruitment and training of CIN team members. This will entail investments in personnel infrastructure needed to navigate all of the complexity and transitions CINs are sure to encounter, both internally and externally.
Key takeaways for CINs ready to lead the next iteration in the transition to value
- Drive institutional understanding of VBC—CIN leaders can take an active role in providing education
- Identify opportunities to integrate CIN strategic planning with health system enterprise strategic planning
- Evaluate and prioritize VBC investment opportunities on the basis of the ROI potential, horizon and even probability of desired impact
- Balance focus on near-term investments in CIN value creation with patience to allow for value capture
- CINs at every stage in the journey can create VBC impact for creating and capturing value
As your organization evaluates CIN strategies at all stages of evolution, reach out to our Value-Based Care Strategy Consulting experts for help with your initiatives and goals.
Related resource: